BBMRI.at & COVID-19
COVID-19 caused by the SARS-CoV-2 corona virus represents a great challenge for our healthcare and economic systems. The situation and the working conditions are difficult in many places and direct patient care has the highest priority.
The Medical University BBMRI.at partners are doing a great job in patient diagnosis, care and treatment. In addition, there are also research activities towards finding ways to deal with the COVID-19 disease. Biobanks can support researchers and provide key services to them, such as:
- Efficient and high-quality storage of samples in clinical and research settings;
- Samples from healthy individuals, to be used as control (collected 2-3 months before outbreak in each country);
- Provide guidance and standards for targeted identification, collection and conservation of important samples.
Med Uni Graz (with Institute of Pathology and Biobank Graz)

Available resources:
- Austria’s highest biosecurity laboratory and autopsy area (BSL-3)
- Access to patient samples
- Isolation of pathogens from autopsy cases (BSL-3)
- SARS-CoV-2 virus culture (BSL-3)
- Sequence characterized SARS-CoV-2 variants isolated from Austrian patients
- Isolated SARS-CoV-2 proteins from various virus variants
- Isolated SARS-CoV-2 RNA quantified by digital PCR
- Inhibitor testing
- Support in diagnostic assay development
Contact: kurt.zatloukal@medunigraz.at
- COVID-19 convalescent cohort (saliva, serum, Li-Hep plasma, EDTA plasma, Na-Citrate plasma, EDTA buffy coat, nasopharyngeal swab; questionnaire on symptoms, 5 visits)
- COVID-19 vaccination cohort (serum, PBMCs, saliva; 5 visits; immunosuppressed and healthy patients)
- Prospective sample collection/study cohorts
Contact: christian.guelly@medunigraz.at
Media reports about the High Security BSL-3 Lab and Biobank Graz contribution to COVID-19 research at Med Uni Graz

- Servus TV report (PM Wissen): “How could drugs against corona help?”
- ORF report: “COVID-19 recovered study showing eight month antibodies in blood”
- RTL TV report: “Anti corona nasal spray with banana protein”
- Servus TV report: “Corona – auf der Suche nach der Wahrheit”
- ORF report: “Tablet against COVID-19 transmission” at universities in Graz
- ORF Steiermark: “Grazer Speziallabor im Einsatz gegen COVID-19”
- Kleine Zeitung: “Med Uni Graz – Speziallabor für hochinfektiöses Material in Graz”
Med Uni Vienna (with MedUni Wien Biobank)

Available resources:
- Serum samples collected before the SARS-CoV-2 outbreak (for validation of serologic (IgG, IgM) tests, as those samples might be definitively free from antibodies against the virus);
- Collections from patients with COVID-19 collected in clinical setting are currently in planning.
- Samples from population-based cohorts collected after the SARS-CoV-2 outbreak (e.g. collected during prophylactic health examination programs, emergency department/primary care visits, etc.) that might help to estimate the actual seroprevalence of the virus in the different areas: COVID-19 convalescent cohort and COVID-19 vaccination cohort
Contact: helmuth.haslacher@meduniwien.ac.at
Media reports:
- ORF report: “Search for participants for CoV “booster” study” with MUW Biobank involvement
- Award for COVID-19 research project with MedUni Wien Biobank involvement
- ORF TV report: “2nd vaccination unnecessary for COVID-19 recovered”
Med Uni Innsbruck (with Biobank Innsbruck)

Available resources:
- Samples from patients with COVID-19 collected in clinical setting from the Tyrol region (Austria COVID-19 hotspot), linked to clinical data.
Contact: georg.goebel@i-med.ac.at; johannes.haybaeck@i-med.ac.at
BBMRI.at experts contributed to the development of an ISO standard for COVID testing that will help to improve testing procedures and contribute to a safer world.
ISO/TS 5798 provides recommendations for the design, development, verification, validation and implementation of analytical tests for detecting the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) using nucleic acid amplification.
ISO/TS 5798:2022, In vitro diagnostic test systems — Requirements and recommendations for detection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by nucleic acid amplification methods
- Available at Austrian Standards (German) and ISO (English)
WHO Laboratory biosafety guidance related to the novel coronavirus – Interim guidance (12 Feb 2020)
Laboratory Biosafety Guidelines for Handling and Processing Specimens Associated with Coronavirus Disease 2019 (COVID-19) – Interim guideline (31 March 2020)
Dealing with COVID-19 contaminated waste: Guideline by Austrian Federal Ministry for Climate Action, Environment, Energy, Mobility, Innovation and Technology (German)
Austria, Styria: “Steirischer Seuchenplan” – requires autopsies to be performed in BSL-3 laboratories
Biospecimens containing SARS-Cov-2:
- Heather A. Lankes, and Hala Makhlou (2020): Biospecimen Collection During the COVID-19 Pandemic Considerations for Biobanking, Am J Clin Pathol 2020;XX:1–0, DOI: 10.1093/AJCP/AQAA171
Key points:
- Current data suggest the earliest cases in the COVID-19 pandemic may have been as early as October 2019.
- Millions of biospecimens have been and will be collected from known and suspected cases, as well as asymptomatic and presymptomatic individuals for various purposes.
- Biosafety considerations intended to complement evolving CDC and WHO guidelines are presented.
- Wenling Wang (11 March 2020): Detection of SARS-CoV-2 in Different Types of Clinical Specimens, JAMA. 2020;323(18):1843–1844, DOI: 10.1001/jama.2020.3786
Key points:
PCR test on specimens from COVID-19 patients with fever, dry cough, and fatigue revealed that the virus was present in the following specimens;
– Highest rates: in bronchoalveolar lavage fluid (14 positive results of 15 samples; 93%),
– followed by sputum (72 of 104; 72%),
– nasal swabs (5 of 8; 63%),
– fibrobronchoscope brush biopsy (6 of 13; 46%),
– pharyngeal swabs (126 of 398; 32%),
– and feces (44 of 153; 29%).
– Lower positive rates were found in and blood (3 of 307; 1%).
– None in urine (0 of 72; 0%).
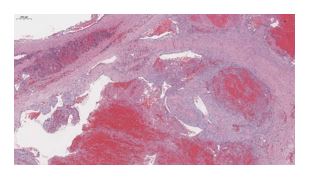
- Anthony F. Henwood (2020): Coronavirus disinfection in histopathology, Journal of Histotechnology, DOI: 10.1080/01478885.2020.1734718
This technical note presents disinfection procedures and histotechnology processes for corona virus containing specimens and using data obtained from similar coronaviruses, e.g. severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS).
- Darnell ME et al. (2004): Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV. J Virol Methods. 2004 Oct 1;121(1):85–91, DOI: 10.1016/j.jviromet.2004.06.006
In older studies on SARS-CoV viruses, it was determined that formalin and glutaraldehyde inactivated SARS-CoV in a temperature- and time-dependent manner. Formalin fixation performed at 37°C or room temperature, “significantly decreased the infectivity of the virus on day 1, while glutaraldehyde inactivated SARS-CoV after incubations of 1–2 days.
- Duan et al. (2003): Stability of SARS coronavirus in human specimens and environment and its sensitivity to heating and UV irradiation. Biomed Environ Sci. 2003 Sep;16(3):246–255.
The authors found that several coronaviruses were made non-infectious after the following exposure times and temperatures: 90 min at 56°C, 60 min at 67°C, and 30 min at 75°C. Paraffin infiltration in most histopathology laboratories uses a temperature of 60–65°C for 2 h or more. It is, therefore, appropriate to consider that the formalin-fixed paraffin-embedded tissue block would have a low risk of coronavirus infectivity.
Covid-19 tests:
- Sheridan C. et al.: Fast, portable tests come online to curb coronavirus pandemic. Nat Biotechnol. 2020 Mar 23, DOI: 10.1038/d41587-020-00010-2